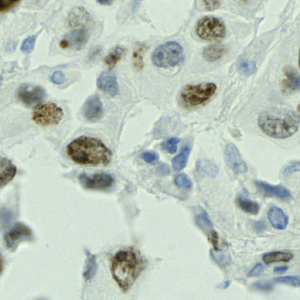
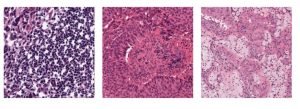
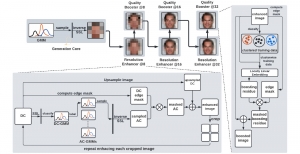
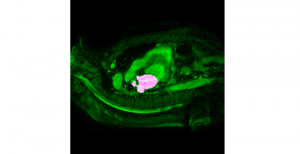
Magnetic Resonance Imaging(MRI) is a non-invasive, radiation-free scanning procedure generally used to obtain images of internal organs. This imaging modality is a popular screening technique for Prostate Cancer. A Prostate MRI may be used to detect prostate cancer, determine the requirement for biopsy, guide needles during targeted MRI biopsy, or detect the spreading of cancer to neighboring areas. Current standards of MRI acquisition still lead to errors, like false detections, where patients are unnecessarily sent to biopsy, or missed detections, where existing tumors remain undetected. A good quality MRI is essential to ensure that Prostate Cancer is diagnosed on time.
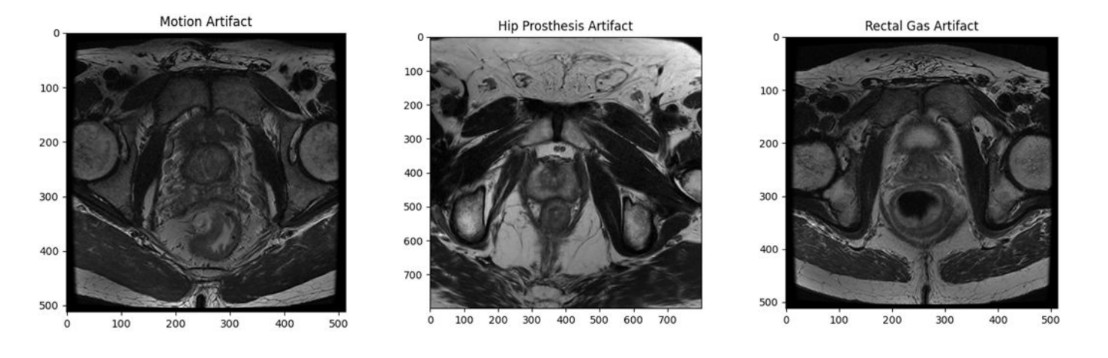
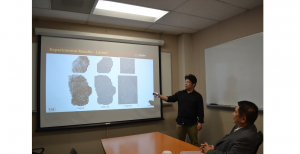
An MRI has several sequences, namely T2W, ADC, and DCE. For an MRI to be of diagnostic quality, atleast two of the three sequences must independently be of diagnostic quality. Errors/artifacts may be present in some or all of these sequences. Some common artifacts include motion artifacts, rectal gas, hip prosthesis, etc., that affect the quality of the MRI.
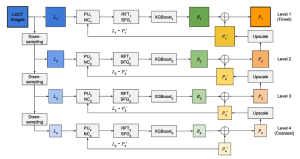
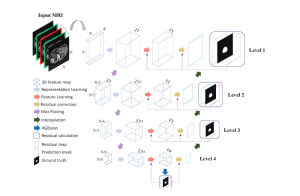
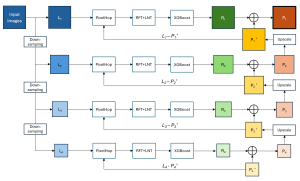
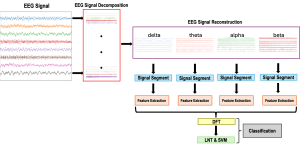
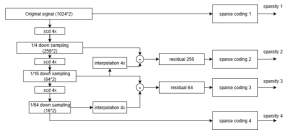
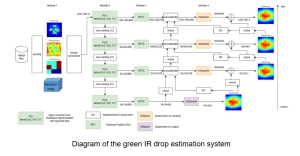
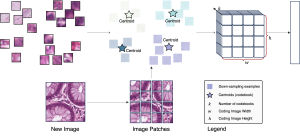
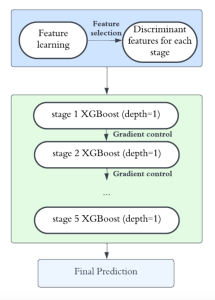
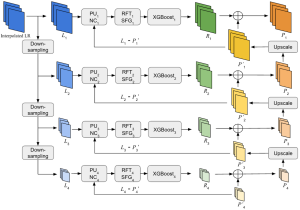
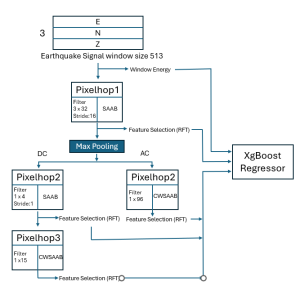
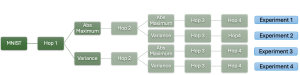
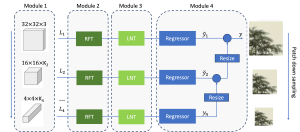
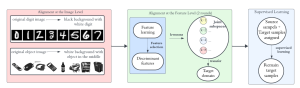
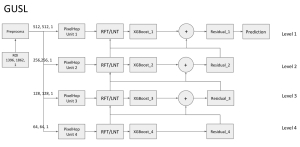
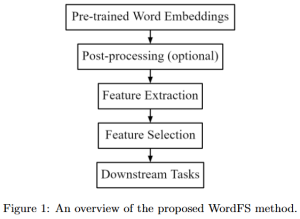
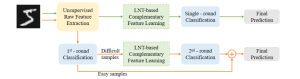
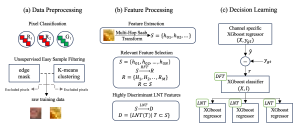
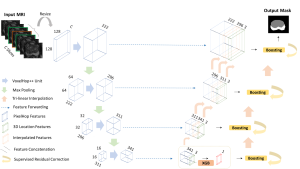
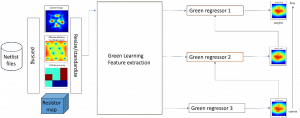
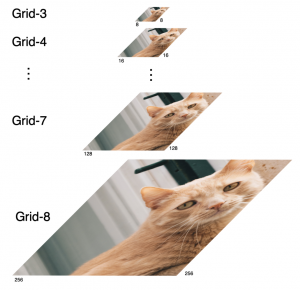
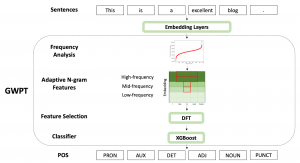
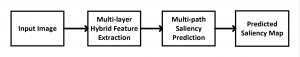
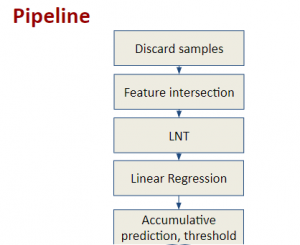
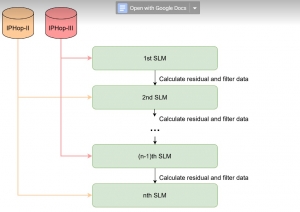
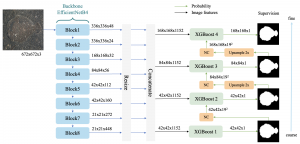
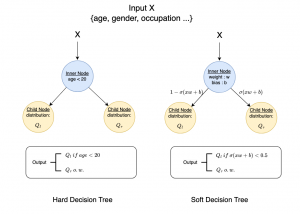
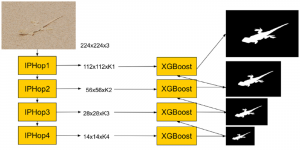
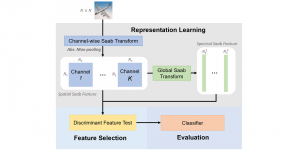
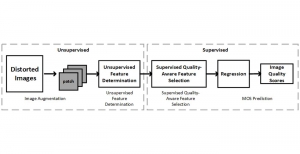
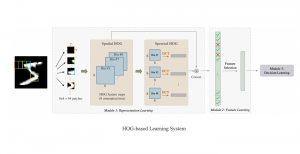
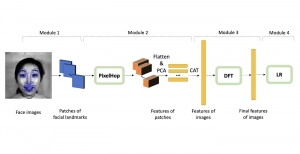
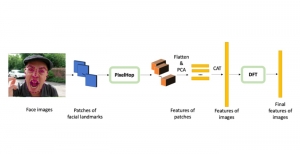
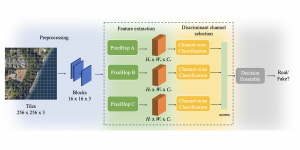
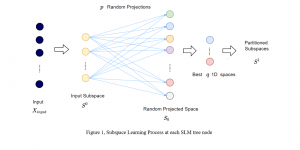
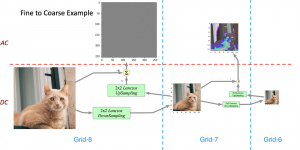
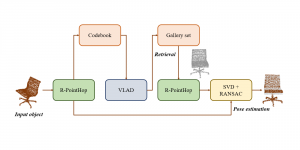
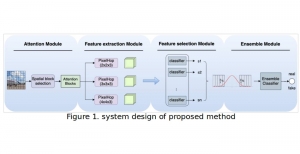
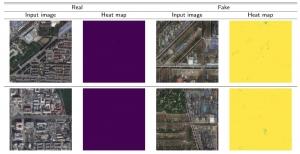
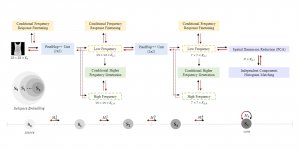
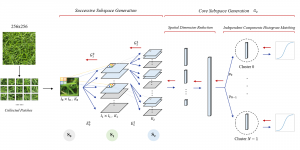
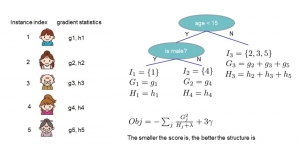
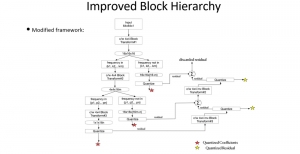
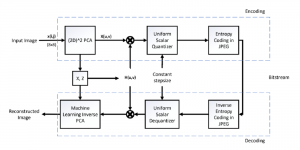
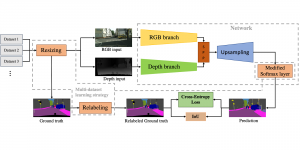
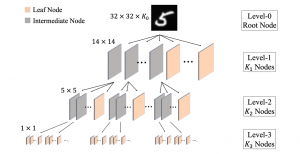
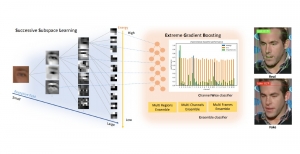
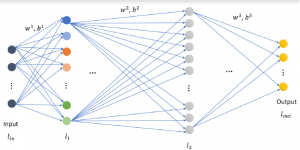
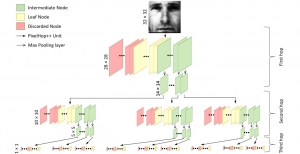
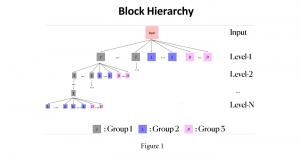
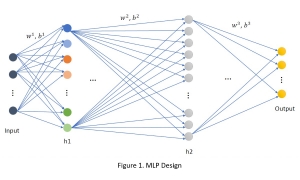
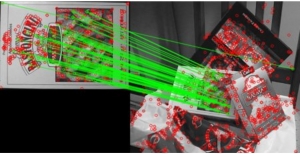
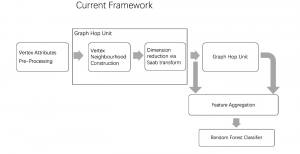
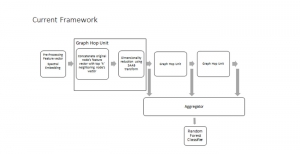
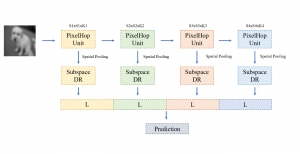
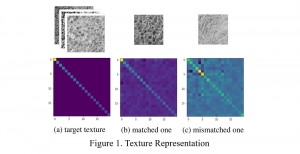
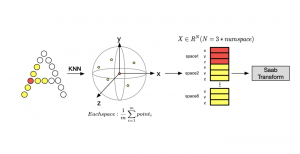
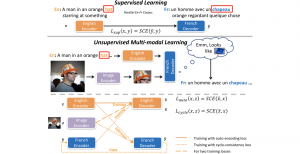
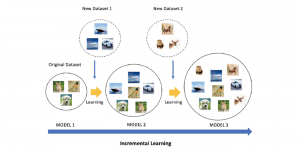
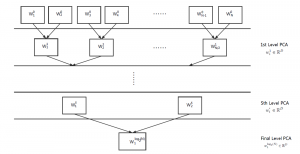
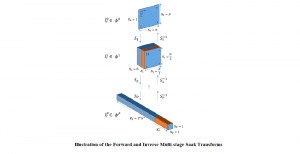
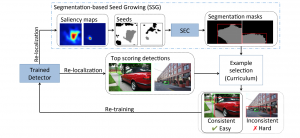
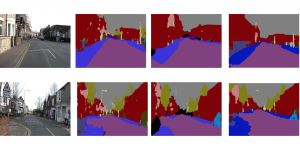
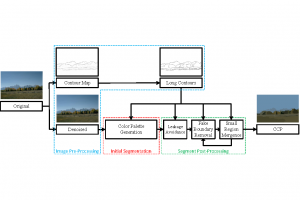
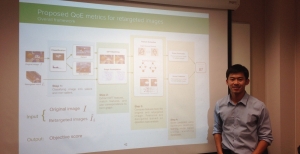
In order to assess the quality of an MRI, we train independent models for each of these sequences. While MRI images are volumetric, we treat each slice of the MRI independently. 2D Haar Wavelet Transform is applied to extract features from the LL, LH, HL, and HH bands. These features are extracted at two different resolutions. The Discriminant Feature Test(DFT) is used to reduce the feature dimension by removing features with a high DFT loss. An XGBoost Classifier is then trained using these selected features to predict whether each slice of the MRI is of satisfactory quality or not. The quality predictions from each of the three sequences are then combined to obtain the final MRI quality prediction. This approach is light-weight, efficient, and explainable, with good performance that can enable preliminary assessment of MRI quality.